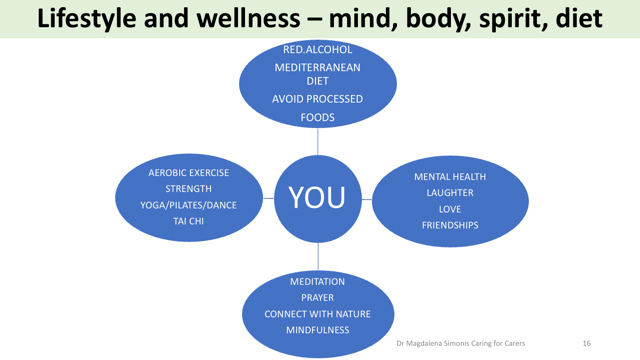
In this RACGP NewsGP article, Assoc Prof Simonis is interviewed to give her perspective on causes of and prevention of ‘doctor burnout’. For AFMW readers she shares a simple graphic she creates for use in her talks on ‘Caring for the Carer’.
RACGP – ‘Burnout twice as risky for patient safety: Study’
A large new meta-analysis also shows burnt out doctors are three times more likely to consider leaving their job or regretting their career.
Burnt out doctors are twice as likely to be associated with patient safety incidents and four times more likely to be dissatisfied with their job, a new comprehensive systematic review and meta-analysis shows.
It also reveals burnt out doctors are three times more likely to consider leaving their job, twice as likely to receive low satisfaction from patients and three times more likely to have regrets about their career.
Published in The BMJ, the research is the largest of its kind to date, and involved an analysis of 170 studies involving 239,246 physicians worldwide.
According to the study, ICU and emergency physicians are most likely to experience burnout, with GPs deemed the lowest risk.
However, Dr Tim Jones – who has spoken openly about his own experiences with burnout – told newsGP that GPs are not immune.
‘GP burnout [is] steadily increasing as workforce shortages and demands across the healthcare sector continue to increase. More of my colleagues [are] leaving GP for more controlled work environments,’ he said.
‘[It’s] still the most meaningful job a doctor can perform but maintaining healthy boundaries with patients [is] getting increasingly critical. We desperately need better support from Medicare to continue high standards of care.
‘In the meantime, I still advocate that if a GP isn’t feeling compassionate for their patients in a healthy way, they are suffering burnout and must take steps to balance their work demands.’
Doctor burnout isn’t new but has been worsened by the demands on healthcare in the era of COVID.
A 2021 Monash University publication noted high levels of psychological distress among Australian frontline workers, with 59% reporting anxiety, 70% with moderate to severe burnout and 57% with depression.
RACGP Expert Committee – Quality Care member Dr Magdalena Simonis, believes COVID has had a profound effect on GPs.
‘We’ve had the Medicare freeze which was worsened by COVID as we were forced to bulk bill for telehealth, while our non-GP specialist colleagues weren’t,’ she told newsGP.
‘GPs have also been left out of strategy [discussions] for managing health in the community, and this heightens dissatisfaction.
‘But the RACGP has responded well by advocating for telehealth and more recently has managed to get [more GP representation] in the DoH.’
Recent high profile cases in relation to doctor burnout include past-RACP President and Alfred Hospital physician Professor John Wilson and past-AMA vice president and emergency physician Dr Stephen Parnis.
The BMJ authors point to ways for improvement.
‘A range of effective interventions for reducing burnout in physicians are available,’ they wrote.
‘[These include] interventions focusing on improving the culture on healthcare organisations, interventions supporting individual physicians through organisational funded initiatives, and multicomponent interventions.’
Dr Simonis points to peer support groups, such as Doctors for Doctors, and other individualised factors to prevent burnout.
‘To be a good doctor, you need to look after yourself,’ she said.
‘For example spending time in nature, exercising, taking time out from office and desk, connecting with friends and maintaining relationships, seeking mental health support, addressing diet and being mindful [can all help].’
However, while individual interventions may help, Dr Tammra Warby, a GP with a PhD in virology says there is a sense that healthcare workers can ‘just deal with it’, and is instead calling for more systemic action.
‘Without healthcare workers, hospitals are just buildings,’ she told newsGP.
‘The conditions that lead to burnout can crossover with those that compromise patient safety. For example, [doctors] working outside of the scope of their practice, constant rapid changes in roles or processes, inadequate staffing, unsafe workplace environment and excess hours.
‘The article recommends implementation of evidence-based practices to improve outcomes, and I agree with this, [which] is why I suggested [a] taskforce who could develop those succinct guidelines.
‘The Mayo clinic does so and implements them.’
Dr Warby recommends a similar taskforce to orchestrate universal guidelines for all doctors, including GPs, which can be adopted for burnout prevention.
‘Organisations need to be accountable for the way they treat healthcare workers,’ she said.
‘The guidelines could be part of accreditation. I think the RACGP, AMA, ANMAC [Australian Nursing and Midwifery Accreditation Council], etcetera need to lead calls on the government and become stakeholders in this kind of taskforce.
‘We need to move from talk to action.’
Source article and photo credit: https://www1.racgp.org.au/newsgp/clinical/burnout-twice-as-risky-for-patient-safety-study
Associate Professor Magdalena Simonis AM is a Past President of the AFMW (2020-2023), former President of VMWS (2013 & 2017-2020) and current AFMW National Coordinator (2024-2026). She is a full time clinician who also holds positions on several not for profit organisations, driven by her passion for bridging gaps across the health sector. She is a leading women’s health expert, keynote speaker, climate change and gender equity advocate and government advisor. Magda is member of The Australian Health Team contributing monthly articles.
Magdalena was awarded a lifetime membership of the RACGP for her contributions which include past chair of Women in General Practice, longstanding contribution to the RACGP Expert Committee Quality Care, the RACGP eHealth Expert Committee. She is regularly invited to comment on primary care research though mainstream and medical media and contributes articles on various health issues through newsGP and other publications.
Magdalena has represented the RACGP at senate enquiries and has worked on several National Health Framework reviews. She is author of the RACGP Guide on Female Genital Cosmetic Surgery and co-reviewer of the RACGP Red Book Women’s Health Chapter, and reviewer of the RACGP White book
Both an RACGP examiner and University examiner, she undertakes general practice research and is a GP Educator with the Safer Families Centre of Research Excellence, which develops education tools to assist the primary care sector identify, respond to and manage family violence . Roles outside of RACGP include the Strategy and Policy Committee for Breast Cancer Network Australia, Board Director of the Melbourne University Teaching Health Clinics and the elected GP representative to the AMA Federal Council. In 2022. she was award the AMA (Vic) Patrick Pritzwald-Steggman Award 2022, which celebrates a doctor who has made an exceptional contribution to the wellbeing of their colleagues and the community and was listed as Women’s Agenda 2022 finalist for Emerging Leader in Health.
Magdalena has presented at the United Nations as part of the Australian Assembly and was appointed the Australian representative to the World Health Organisation, World Assembly on COVID 19, by the Medical Women’s International Association (MWIA) in 2021. In 2023, A/Professor Simonis was included on the King’s COVID-19 Champion’s list and was also awarded a Member (AM) in the General Division for significant service to medicine through a range of roles and to women’s health.